Throughout the world – and here in New Zealand – a pervasive and persistent care gap exists for people suffering fragility fractures caused by osteoporosis. The International Osteoporosis Foundation (IOF) has collated numerous studies conducted at the international, national, regional and local level which demonstrate that a minority of fragility fracture sufferers receive the secondary preventive care that they need. Given that those who suffer fractures are at double the risk of suffering subsequent fractures compared to their peers who are fracture free, and that half of patients who suffer hip fractures break another bone before breaking their hip, this is a missed opportunity that New Zealand cannot afford.
In response to this, Osteoporosis NZ has worked with the Ministry of Health, Health Quality & Safety Commission New Zealand (HQSC) and other key stakeholders to drive implementation of Fracture Liaison Services (FLS) by all District Health Boards (DHBs) in New Zealand. In December 2014, Osteoporosis NZ has published a FLS Resource Pack, with the intention of supporting those DHBs which are yet to implement a FLS, in accordance with the requirement of the 2014-15 District Annual Planning guidance from the Ministry of Health. Click to download the FLS Resource Pack – which has been endorsed by HQSC. Microsoft Word versions of several appendices 2-5 – including a fully-referenced FLS business plan template – can be downloaded from the Fracture Liaison Service Resource Pack page.
In a growing number of countries FLS have been shown to eliminate the post-fracture care gap in a highly cost-effective fashion. Case studies describing the recently established Waitemata FLS and several well-established FLS from overseas can be viewed from the links below:
United States of America
Kaiser Permanente Healthy Bones Program
Over the last 15 years, the Kaiser Permanente Healthy Bones Program has grown to become one of the most successful fracture prevention initiatives in the world. In 2007, it was estimated that the program prevented 970 hip fractures among the 3.2 million members of Kaiser Permanente in Southern California. Since launching in 1998, the Healthy Bones Program has led to an overall 38% reduction in the expected hip fracture rate.
At the outset, the Healthy Bones Program aimed to reduce the incidence of hip fractures by 25%. The Plan-Do-Study-Act rapid cycle process improvement methodology was employed to drive continuous quality improvement:
Plan
- Build a team led by a champion
- Set a goal
- Identify patients at risk for a hip fracture
- Risk stratify the population – build the ‘work list’
Do
- Ensure that work is done by the right person at the right time. When a care gap is found, someone must close that care gap. Care managers ‘work the list’ at Kaiser Permanente
Study
- Measure the work done
- Look for variation and make improvements by adapting/adopting good ideas from elsewhere
Act
- Establish a system of incentives and/or sanctions. High quality care is linked to higher remuneration
- Iterate the process until the goal is achieved
- Establish higher goals when initial goals have been achieved
All 13 Kaiser centres in Southern California achieved Gold status from the International Osteoporosis Foundation’s Capture the Fracture Campaign.
The Kaiser team are also the current Guinness World Record holders for the number of DXA scans done in one day at multiple venues!
Read more at:
Agency for Healthcare Research and Quality Service Delivery Innovation Profile for Kaiser Permanente Healthy Bones Program.
Ten Strategies To Lower Costs, Improve Quality, And Engage Patients: The View From Leading Health System CEOs. Cosgrove DM, Fisher M, Gabow P, Gottlieb G, Halvorson GC, James BC, Kaplan GS, Perlin JB, Petzel R, Steele GD, Toussaint JS. Health Aff (Millwood). 2013 Feb;32(2):321-327. PubMed ID 23381525
Fracture prevention in Kaiser Permanente Southern California. Dell R. Osteoporos Int. 2011 Aug;22 Suppl 3:457-460. PubMed 21847765
United Kingdom
The Glasgow Fracture Liaison Service, Scotland
First developed in 1999, the Glasgow FLS is a system to ensure fracture risk assessment, and treatment where appropriate, is delivered to all patients with fragility fractures. The FLS is a ‘doctor light’ service and is primarily delivered by clinical nurse specialists, who work to pre-agreed protocols to case-find and assess fracture patients. Consultant Endocrinologists provide medical leadership for the Glasgow FLS. A critical success factor in development of the Glasgow FLS was establishment of a multi-disciplinary stakeholder group from project outset, with representation from all relevant hospital specialities, local primary care and regional health authority and administrative groups.
The structure of the Glasgow Fracture Liaison Service
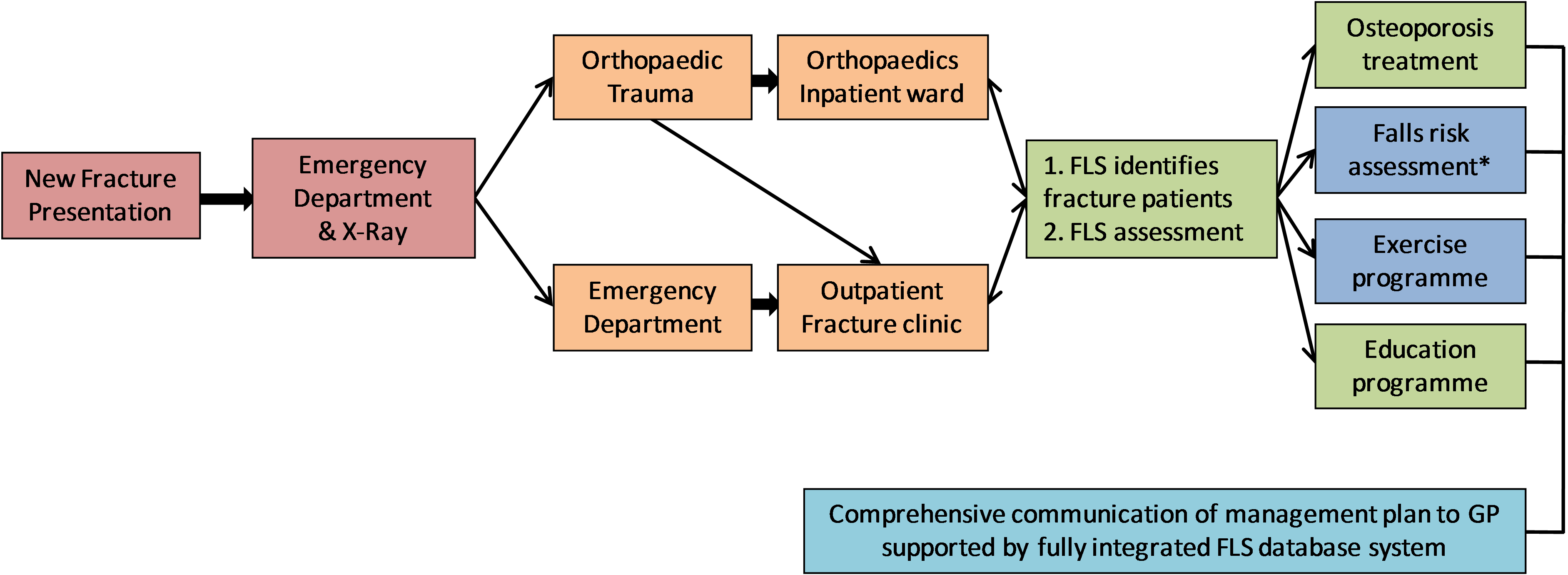
* Older patients, where appropriate, are identified and referred for falls assessment
During the first 18 months of operations:
- More than 4,600 patients with fractures of the hip, wrist, upper arm, ankle, foot, hand and other sites were seen by Fracture Liaison Nurse Specialists
- Nearly three-quarters were considered for BMD testing and treatment was recommended for approximately 20% of patients without the need for BMD testing
- 82% of patients tested were found to be osteopenic or osteoporotic at the hip or spine
During the first decade of this century over 50,000 consecutive fracture patients have been assessed by the Glasgow FLS. During this period, hip fracture rates in Glasgow have been reduced by 7.3% versus almost a 17% increase in England, where only 37% of localities operated a FLS by late 2010. A Scottish national audit compared case ascertainment for hip and wrist fractures in Glasgow versus 5 other centers operating less systematic models of care. Ninety-seven percent of hip fracture and 95% of wrist fracture patients were assessed by the Glasgow FLS versus less than 30% for other service configurations. In May 2011, a formal cost-effectiveness analysis of the Glasgow FLS was published. This study concluded that 18 fractures were prevented, including 11 hip fractures, and £21,000 was saved per 1,000 patients managed by the Glasgow FLS versus ‘usual care’ in the United Kingdom.
Read more at:
The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. McLellan AR, Gallacher SJ, Fraser M, McQuillian C. Osteoporos Int. 2003 Dec;14(12):1028-1034. PubMed ID 14600804
Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. McLellan AR, Wolowacz SE, Zimovetz EA, Beard SM, Lock S, McCrink L, Adekunle F, Roberts D. Osteoporos Int. 2011 Jul;22(7):2083-2098. PubMed ID 21607809
Canada
Osteoporosis Exemplary Care Program, St. Michael’s Hospital, Toronto
In 2002, the orthopaedic unit at St. Michael’s Hospital in Toronto hired an osteoporosis coordinator to identify patients with a fragility fracture and to coordinate their education, assessment, referral, and treatment of underlying osteoporosis. The Osteoporosis Exemplary Care Program (OECP) provided secondary preventive care to fracture patients managed in both the in- and out-patient settings.
Four hundred and thirty fracture patients were evaluated during the first year of operations (276 out-patients and 154 in-patients). Almost all (96%) of these patients received appropriate osteoporosis care:
- 80 out-patients (36%) were treated for osteoporosis prior to assessment by the OECP
- 124 out-patients (56%) were referred to the Metabolic Bone Disease Clinic or to their GP for osteoporosis treatment
- 31% of the 128 in-patients were treated for osteoporosis prior to assessment by the OECP
- Treatment was initiated for a further 24% of in-patients and another 34% were referred to the Metabolic Bone Disease Clinic or their GP for post-discharge consultation on osteoporosis treatment
A cost-effectiveness analysis of the OECP concluded that a hospital that hired an osteoporosis coordinator who manages 500 patients with fragility fractures annually could reduce the number of subsequent hip fractures from 34 to 31 in the first year, with a net hospital cost savings of CN$48,950 (Canadian dollars in year 2004 values), with use of conservative assumptions. Sensitivity analysis indicated a 90% probability that hiring a coordinator costs less than CN$25,000 per hip fracture avoided. Hiring a coordinator is a cost-saving measure even when the coordinator manages as few as 350 patients annually. Greater savings were anticipated after the first year and when additional costs such as rehabilitation and dependency costs are considered.
Read more at:
Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. Bogoch ER, Elliot-Gibson V, Beaton DE, Jamal SA, Josse RG, Murray TM. J Bone Joint Surg Am. 2006 Jan;88(1):25-34. PubMed ID 16391246
A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs. Sander B, Elliot-Gibson V, Beaton DE, Bogoch ER, Maetzel A. J Bone Joint Surg Am. 2008 Jun;90(6):1197-1205. PubMed ID 18519311
Australia
Minimal Trauma Fracture Liaison (MTFL) Service, Concord Repatriation General Hospital, Sydney
The Minimal Trauma Fracture Liaison (MTFL) service was established in 2005 at this large tertiary referral centre in Sydney. The MTFL service provides a good illustration of effective collaboration between a physician-led FLS and the hospital’s Orthogeriatrics Service (akin to Geriatric Fracture Center models in the United States); the MTFL provides care for non-frail patients with fragility fractures whilst the Orthogeriatrics Service focuses on frail patients, including the majority of hip fractures. The MTFL is delivered by an advanced trainee (i.e. a physician in his/her 4th-6th year of post-graduate training) which required a 0.4-0.5 FTE appointment.
The impact of the MTFL service was evaluated after 4 years. Fracture patients who chose to decline the consultation freely offered by the service, in favour of follow-up with their primary care physician, were considered as a control group for statistical comparison. Refracture incidence for those patients managed by the MTFL service was 80% lower than the control group. A published cost-effectiveness analysis of the MTFL service reported:
- A mean improvement in discounted quality-adjusted life expectancy per patient of 0.089 QALY gained
- Partial offset of the higher costs of the MTFL service by a decrease in subsequent fractures, which lead to an overall discounted cost increase of AU$1,486 per patient over the 10-year simulation period
- The incremental costs per QALY gained (incremental cost-effectiveness ratio – ICER) were AU$17,291, which is well below the Australian accepted maximum willingness to pay for one QALY gained of AU$50,000
Read more at:
Targeted intervention reduces refracture rates in patients with incident non-vertebral osteoporotic fractures: a 4-year prospective controlled study. Lih A, Nandapalan H, Kim M, Yap C, Lee P, Ganda K, Seibel MJ. Osteoporos Int. 2011 Mar;22(3):849-858. PubMed ID 21107534
Cost-effectiveness of the Concord Minimal Trauma Fracture Liaison service, a prospective, controlled fracture prevention study. Cooper MS, Palmer AJ, Seibel MJ. Osteoporos Int. 2012 Jan;23(1):97-107. PubMed ID 21953475
Waitemata FLS
This case study was kindly drafted by Dr. David Kim of Waitemata DHB.
The Waitemata DHB Fracture Liaison Service (FLS) was established in late 2012 after a period of careful planning by a coalition of multi-department representatives. The aim of developing our FLS was to prevent fractures in those at highest risk of future fractures, by capturing fragility fractures presenting to our hospitals and implementing appropriate assessment and treatment for osteoporosis. The project was initially led by Dr. Joe Singh, Geriatrician, with a guiding support from Paul Mitchell, Acting Chair of Osteoporosis New Zealand with his extensive knowledge and experience with FLS abroad. We were also fortunate to have research grant from Merck Sharp & Dohme (MSD) to fund 0.5 FTE Fracture Liaison Nurse, and were the first DHB to have dedicated FLS nurse.
Our inaugural fracture liaison nurse was Maria Harrison who, with the oversight of Dr. Joe Singh, was instrumental in setting up the infrastructure for the service in 2012 and 2013. Endocrinology department, led by Dr. Rick Cutfield, provided extra bone mineral density (DXA) scans for the FLS implementation. Regular multidisciplinary meetings were held with presence of relevant representatives from various subspecialties (Older People’s Health, Endocrinology, Orthopaedics and Emergency Medicine). Endocrinology Service Manager, Brian Millen, has been regularly and intimately involved with FLS work throughout. We successfully secured DHB funding in 2013 for ongoing FLS at WDHB.
In 2013, we started capturing fragility fracture cases, some from inpatient wards but, mainly from Orthopaedic fracture clinic. One hundred and sixty cases were captured in 2013, with the majority being fractures of the wrist and humerus, but also some vertebrae, hip, and ankle fractures. Laboratory investigations were done and DXA was performed in selected cases, with appropriate therapy started or recommended. Our service attained the ‘Bronze’ status from the International Osteoporosis Foundation’s Capture the Fracture® Campaign on the basis of our 2013 work.

There was a change of team at the end of 2013. Denise MacKenzie was appointed as our new FLS nurse and Dr. David Kim, Endocrinologist, as the lead clinician. A protocol was fine-tuned for implementation of more systematic and streamlined case detection, assessment and treatment. We are continuing to capture those over the age of 50 years with fragility fracture from the fracture clinic, but are now detecting a lot more inpatient cases, especially the hip fractures. All captured patients are either seen or contacted via a phone call by Denise. She explains the role of FLS to the patient and offer appropriate screening. All agreeable patients go through selected laboratory investigations, and a large proportion of patients have DXA (those aged between 50 and 75 years) to aid treatment decision. After completion of the assessment, each individual’s case is discussed by Denise and Dr. Kim, and a brief clinical letter is addressed to the patient’s GP. Complex cases, especially those with recurrent or multiple fragility fractures, are arranged to be seen in Endocrine outpatient clinic.

Going forward, we would like to continue to develop and grow our service. We are looking at opportunities for additional funding to increase FLS co-ordinator time, as we are currently unable to capture a significant proportion of fragility fractures at our two hospitals. We are currently working on systematic capture of larger number of fracture patients via clinical coding and radiology. We are actively planning to appoint a dedicated falls prevention programme with a FLS Physiotherapist.
With our experience thus far, we believe that following are the key elements in successful FLS establishment and implementation:
- Engaging DHB management/leadership early to secure funding and support
- Gathering interested parties from various subspecialties of the DHB with regular and formal planning meeting
- Having a ready access to funded DXA scans
- Clearly defining the target population, means of capturing cases, protocol for evaluation and treatment implementation
- Active and regular clinician input with the FLS co-ordinator for management decisions
Active and regular clinician input with the FLS co-ordinator for management decisions
Other leading FLS initiatives
The IOF has invested considerable resources into development of the Capture the Fracture® Campaign. This includes development of a set of standards against which FLS can be benchmarked internationally, the Best Practice Framework. Osteoporosis Canada and the National Bone Health Alliance (NBHA) in the United States have developed major FLS and secondary fracture prevention initiatives. Details are available from:
- International Osteoporosis Foundation: The Capture the Fracture Campaign is leading the global drive for implementation of FLS.
- National Bone Health Alliance (U.S.A.): The Fracture Prevention CENTRAL website and associated webinar program and 2Million2Many Campaign are components of the NBHA’s ‘20/20 Vision’ which aims to reduce the incidence of fragility fractures by 20% in the United States by year 2020.
- Osteoporosis Canada: The Make the FIRST break the LAST with Fracture Liaison Services initiative calls for all jurisdictions in Canada to implement an FLS by 2015.





 Print
Print